Last night at the Public Safety Review Committee we heard a report from the Fire Department on their research and recommendations/thoughts.
WATCH IT
If you want to watch it, the video will be here eventually. It was at least 2 and probably more like 3 hours into the meeting.
PROJECTED COSTS
They were very clear that nothing has been decided, this is for 24/7 service. They have also talked about having 12 hours of service as well. Generally they said it would cost $700,000 = $1M. Also, there is a question about if the mental health providers would be City of Madison employees or contracted through a provider like Journey Mental Health. I vote for City of Madison employees with benefits. They discussed how it is difficult to keep mental health providers in our community due to the low pay. I think making them City employees would help.
Crisis Response Team Projected Cost Summary:
1) Annual Salary and Benefits
a) Four full-time community paramedic positions: $327,000 (approximate based on City of Madison CG16, RG15)
b) Four full-time mental health provider positions: $280,000 (approximate based on U.S. Bureau of Labor Statistics for Dane County)
c) One part-time Mental Health Medical Director: $70,000 (approximate based on half-time rate according to U.S. BLS for Dane County)
d) Estimated Annual Total: $677,000
2) One Time Start-up Costs
a) Vehicle: $48,000 (electric Ford Explorer)
b) Radios: $8,900 (one mobile and two portable radios)
c) Vehicle router: $1,300
d) AED and medical supplies: $5,000
e) Computer hardware: $7,000 (two tablets)
f) Uniform/clothing: $2,000 ($500 x 4 for community paramedics only)
g) Cell phone: $1,000
h) Office supplies: $200
i) Estimated Total: $73,400
THE REPORT
A few things we learned last night not in the report is that in the CAHOOTS program in Eugene Oregon they had 24,000 calls – I believe in 2019 – and they only needed to call the police for 250 of them. Also, they anticipate that the calls they would take would be the “welfare checks” that the police are called to. These responders would not be in uniform or have badges of any kind and won’t use lights and sirens. The working title is CARE (Community Alternative Response to Emergencies). Here’s the printable report: Crisis Response Team Draft
Executive Summary
In 2019, over 3000 people accessed crisis mental health services in Dane County. Several City of Madison agencies have been tasked with reviewing the current mental health crisis response model while providing recommendations aimed at improving overall patient outcomes. In researching national best-practices around mental health response, the model found to be most patient-centered is one that incorporates first responders with mental health providers. Currently the City of Madison’s mental health crisis response model is primarily law-enforcement driven with no 24/7 mental health facility available. In order to develop additional services to reduce gaps in crisis care, this paper supports the following recommendations:
- Develop a 24/7 Crisis Response Team that incorporates specially trained community paramedics with mental health providers.
- Annual cost estimate: $700,000 to $1,000,000 for staff of four community paramedics, four mental health providers and one mental health medical director.
- Initial cost estimate: $75,000 one-time cost for a vehicle, technology, radios and medical equipment will be necessary.
- Establish formal partnerships within the local mental health community to assist in treating and diverting mental health patients away from emergency departments and jails.
- Develop triage protocols to be used by the 9-1-1 Center and emergency responders to recognize appropriate and safe situations for deployment of the Crisis Response Team.
Introduction
People experiencing a mental health crisis receive variable and poorer quality care than those experiencing a physical health crisis. Cities all across the United States are missing opportunities to provide better care to this population and in potentially avoidable mortality, morbidity, and service burden. Developing and testing interventions for this patient group in pre-hospital settings could lead to reductions in suicide, patient distress, and service usage throughout Dane County.
The high levels of patient repeat mental health emergency calls, and frequency of self-discharges from Emergency Departments further emphasize the importance of developing evidence-based interventions to improve outcomes and reduce service burden. These findings may be explained by qualitative research that suggests that people who experience a psychiatric emergency or have self-harmed often feel that their needs are not met by responding police officers and even within an Emergency Department.
Suicide is a leading cause of death in young people and a globally significant public health concern. The Crisis Response Team (CRT) therefore has a unique opportunity to deliver a range of potential suicide prevention strategies through developing alternative care pathways to specialist mental health services, delivering suicide prevention interventions, and registering risk of suicide on admission to the Emergency Department.
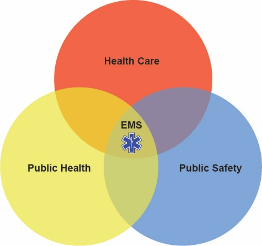
Modern EMS is a combination of public health, public safety, and health care.
Dane County EMS agencies reported a 46% increase in alcohol/substance abuse calls in the first quarter of 2020 compared to Q1 2019. Even prior to the pandemic, a proportion of patients treated by EMS refused transport to the emergency room, where they would have been offered recovery coaching support and medical services. All indications are that patients who refuse transfer:
- 1) are poor, homeless, or afraid they can’t afford ambulance fees or hospital charges;
- 2) may want to avoid interaction with authorities (PD), a factor that the heightened climate of mistrust could exacerbate;
- 3) are disoriented and want to leave as soon as they are revived.
Each of these cases represents a missed opportunity we seek to address through this project. The Crisis Response Team Pilot Project is an extension of work that is already in operation via partnerships that have been coordinated. Dane County Executive Parisi and area EMS agencies have approached Safe Communities about expanding recovery coaching services to this lost population who, without an opportunity to access the support they need, are at high risk of another overdose, triggering more EMS calls, more ED admissions, more jail stays and tragically, more death. Research on recovery coaching and peer support has demonstrated reduction in all these negative outcomes. This Crisis Response Team’s mission will be to prevent unintentional injury with the focus on mental health.
The development of a Crisis Response Team would include one specially trained mental health paramedic and one mental health professional. They would respond in a non-ambulance type vehicle that would be staffed every day for an entire 24-hour period. Calls for service could come from the 9-1-1 Center, on-site emergency crews, the Safe Communities new call center or future community mental health triage centers. A traditional response may be initiated (which could include law enforcement only if needed). In this case the first responders would make an assessment and if the patient’s condition fits the scope of practice, the Crisis Response Team would get activated. Once the Crisis Response Team is on scene, the patient would receive specific care dealing with mental health emergencies.
The goal of this plan is to provide an initial front-line medical response to the mental health needs in the community. In order to maximize our capacity to identify patients that may benefit from this type of response, we will need to integrate a more effective triage call method in the 9-1-1 Center. The focus of the response will be for mental health related non-violent calls such as suicidal ideation, check-welfare, abnormal behavior, anxiety and depression.
Additional funding is needed to execute this expansion and staff the Crisis Response Team with specially trained paramedics, a mental health professional, and a Medical Director (focused on mental health). An estimate of annual operating costs is $1 million – $1.5 million, which will cover the salaries of four community paramedics, four mental health professionals, a mental health medical director, and any other associated costs. Also, an estimated $75,000 one-time set-up cost for a vehicle, technology, radios and medical equipment will be necessary.
Paramedics are being called to address patients’ mental health concerns. Current debates around increasing mental health call volume for paramedics, in the media as well as in academia, identify several factors as problematic, such as inappropriate use of paramedic services for mental health and other psychosocial issues, insufficient paramedic mental health training, and deficiencies in community mental health services.
KEY FINDING #1
Paramedics are often a first point of access to the health care system, and one of few health professionals who encounter patients in their everyday settings. Paramedics encounter patients from diverse socio-economic backgrounds and may be a patient’s only access to health care. Although their interventions are usually responses to identifiable medical conditions, there exists a great variety of nonmedical, often labeled “psychosocial,” situations to be managed in the prehospital setting, as well as information to be gained from this exposure. Among situations resulting in calls to paramedic services, “mental health calls” are increasingly frequent and these patients are identified as repeat users of prehospital ambulance care.
KEY FINDING #2
The major key to a successful team is dependent on partnerships. Some essential groups are listed below:
- Public Health Madison and Dane County
- Medical Direction
- Journey Mental Health
- Madison Fire
- Safe Communities: Two months ago, in response to closure of local emergency rooms and Dane County Jail because of the coronavirus, Safe Communities launched a 24-7 Recovery Coach Helpline. A recovery coach is on-call at all times now, and is available to respond to a call from EMS in the field as easily as one from an emergency room. A grant proposal was awarded.
- Local Hospitals (with telehealth)
- City Community Development Office
- City Housing Authority
- Mayor’s Office
- Elected Officials
- Madison Police Department
- Dane County 9-1-1 Center
KEY FINDING #3
A purposive sample of articles illustrates the dominant narrative around paramedicine and mental health calls in the media. One recurring theme is the issue of high, as well as increasing, volume of mental health calls. For instance, one article informs readers that mental health calls make up more than 40% of ambulance runs, another that mental health calls make up the bulk of paramedic calls, and yet another that there is an “aspect” of mental health crisis in every call. These articles suggest that the number of mental health calls is greater than it was in the past, thus burdensome on many community services. In addition, the media refer to mental health calls as a “misuse” of the emergency medical service system. Another recurring theme is the need for more and better mental health training for paramedics. Indeed, paramedics are said to have minimal mental health training and it is generally felt that they would benefit from more. One Madison paramedic states that much of her knowledge of managing mental health calls comes from experience on the road rather than professional training. Most paramedic training currently involves physical findings on assessment, whereas physical findings are largely nonexistent in mental health calls. It therefore suggests that more mental health training may benefit the mental health of patients as well as paramedics themselves. It is essential to the Critical Response Team’s success to have a Mental Health Director to oversee the operation section as well as the training component.
Yet another theme is the need for more mental health services in the community. Dane County is in need of an establishment of a 24-hour crisis center for those struggling with mental health and addictions, and is also calling for more therapists. An article on Thunder Bay, the Canadian city with the highest number of mental health calls per capita in the province of Ontario, states that more paramedics and ambulances will not solve the problem of increasing mental health emergencies, and calls instead for a more holistic approach to the problem, as well as for greater government funding for community mental health services. It is clear that the Madison Fire Department should be a key player in the concept of a Crisis Response Team, however the success relies on City support and other community partners.
Conclusion
Paramedics frequently care for patients who have mental health and/or alcohol and other drug (AOD) problems, which represent a substantial part of their workload. The results indicated that paramedics viewed their role as primarily one of transportation in this situation; they felt ill-prepared to manage and care for these patients, and needed tailored education. There is no argument for the need for deinstitutionalization of mental health care. The Crisis Response Team would fill the gap between health resources while maintaining high-quality health care at a reasonable cost to the patient. The team would advocate for every patient to ensure they receive the best possible care regardless of the ability to pay or insurance status (current racial disparities). This is the time for the City of Madison community to invest in services for all people with mental health and/or AOD problems. One way of responding to the increasing demand of mental health emergencies is to establish a paramedic sub-service (Crisis Response Team) specifically to provide care for people with these illnesses.
Key Take Aways
- The Crisis Response Team will have a unique opportunity to target an identifiably vulnerable cohort and deliver a range of potential prevention strategies that could result in a meaningful decrease in suicides, overdoses, and other mental health emergencies.
- Paramedics on the Crisis Response Team will need more in-service education about the care of patients with mental health and/or AOD problems, and to address concerns about extending their scope of practice to include education with these patients. Thought should be given to introducing current community paramedicine, with a focus on supporting people in the community with mental health and/or AOD problems. There is a need for a change in the City of Madison workplace and organizational culture about scope of practice in caring for patients with these problems. Extending paramedics’ role could, potentially, benefit people with these problems by improving the quality of care, reducing the need for transportation to emergency departments, and decreasing clinicians’ workloads in these departments.
- The Crisis Response Team will need to focus on engaging with mental health service users to share their recovery narratives which will reduce stigma, facilitate healing, and promote engagement in mental health This will provide adequate preparation for service users, accommodate diversity of recovery experiences, be transparent regarding co-creation of narratives, attend to context, and ensure that recovery narratives are never prerequisites for discharge or other clinical decisions.
- The Crisis Response Team will provide psychosocial care in response to a rise in mental health call volume. This proposed program will be a solution to better triaging of patients, better mental health training of paramedics, and promote a need for a greater number of community mental health services. Despite the well-intentioned nature of current solutions, the Crisis Response Team will help shift attention and accountability away from relevant public policies, as well as from broader economic, social, and political determinants of mental health, while placing responsibility on those requiring services or, at best, on the health care system.
- We also argue that the perspective of paramedics, who are exposed to, and interact with, individuals in their everyday environments, has the potential to inform a better, structural and critical, understanding of the factors driving the rise in psychosocial crises in the first place.
- A greater engagement with the political and social determinants of mental health would lead to preventing, rather than primarily reacting to, these crises after the fact.